Project completed as part of the South Health Campus, Alberta Health Services Green Team Competition, 2024
Team members:
Megan Yaraskavitch: Physician Lead, General Neurology Program and Neurology Central Access and Triage, Quality Improvement Lead, Division of Neurology, Clinical Associate Professor, University of Calgary
Vikram Karnik. Site lead, Clinical Neurosciences, South Health Campus, Director, Adult Neurology Residency Program, Clinical Assistant Professor, University of Calgary
Setting / patient group:
General Neurology Clinic. Outpatient follow up appointments for patients with a diagnosis of “migraine”, “headache”, “other migraine”, and “epilepsy”.
Issue:
Emissions caused by transportation to and from the clinic can be quite significant, especially in a city with relatively poor public transport, and at a site that serves a large catchment area with potentially long travel distances to attend. Time spent traveling to and from appointments and in the waiting room can often be longer than the appointment itself. Appointment times are generally longer meaning fewer patients can be seen, and at our centre, 7.4% of in person follow-ups were not attended, whereas only 5.0% of virtual visits were “no shows”. In person appointments also require Nursing and clerical staff.
Intervention
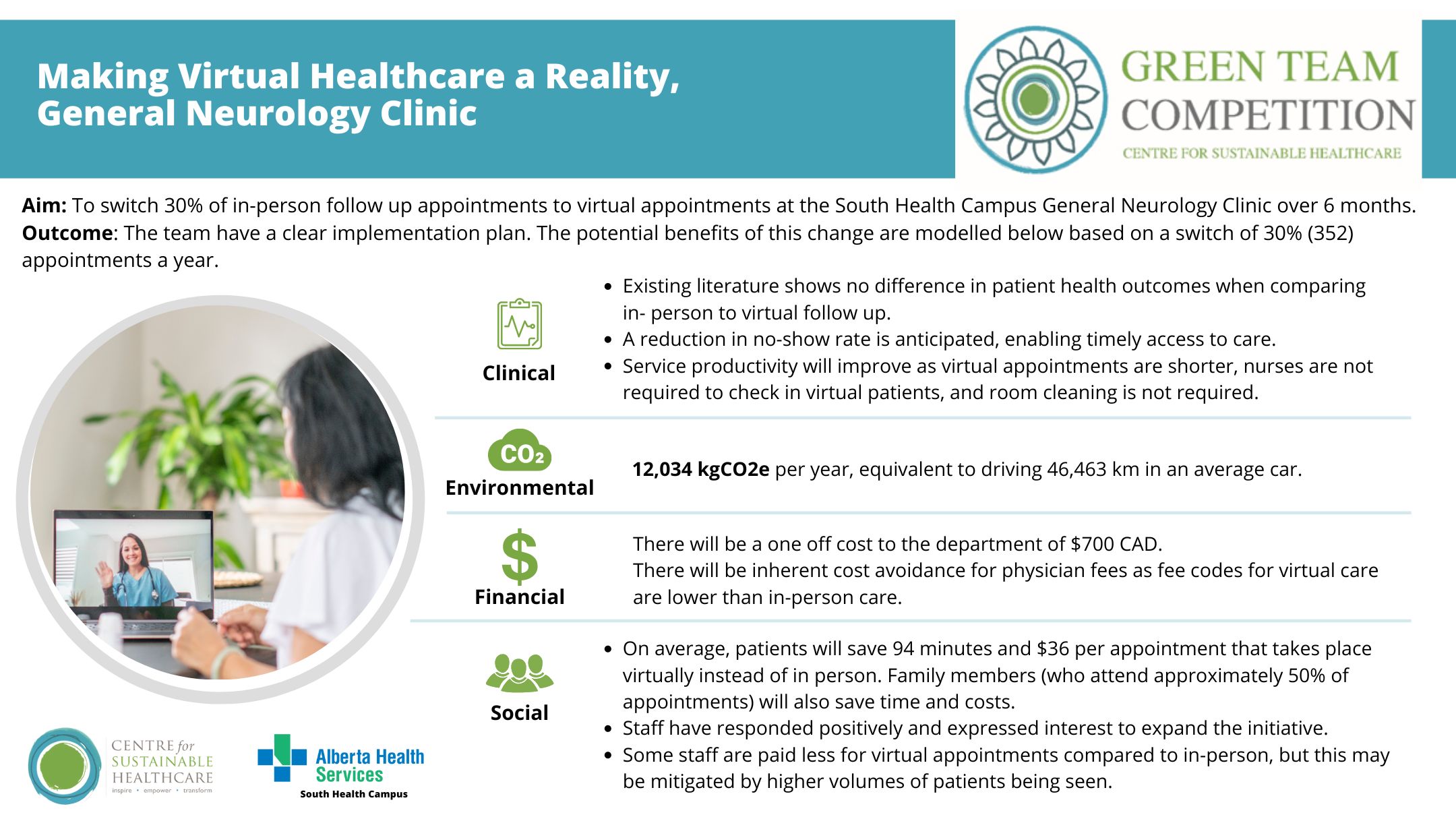
To reduce the number of in-person follow up appointments at the South Health Campus General Neurology Clinic by 30% over 6 months, leading to long term ecological, social, and financial benefit to patients and the healthcare system.
Outcomes
The team extrapolated the potential benefits prior to implementation.
Patient outcomes: We also anticipate a reduction in no-show rate, which may in turn improve patient outcomes and access to care.
Environmental sustainability: It is estimated that if 30% in person visits are replaced with virtual appointments (352 appointments), 12,034 kgCO2e per year would be saved, equivalent to driving 46,463 km in an average car.
Economic sustainability: The project had a once off cost of $700 CAD for equipment. There is an inherent cost avoidance as fee codes for virtual care are less than that of an in-person assessment.
Social sustainability: Patients will save money on fuel, parking and meal costs and gain back approximately one hour of time. Family members attended half of the appointments and would save similar amounts in terms of time and costs. While we have not formally surveyed staff, there has been a lot of positive energy towards this project in preliminary physicians meetings. There were several physicians keen on expanding this initiative beyond just the general neurology clinic.
Key learning point
A key driver to the success of the project was the motivation of the physician group to do “something” to make our healthcare system more sustainable. The hope is that by starting small, we can measure the impact more easily, creating a case to expand to other areas within our department.
Please log in or sign up to comment.