Project completed as part of the Green Nursing Challenge 2025, by the team from Norfolk & Norwich University NHS Foundation Trust.
Team Members:
Phillipa Noble, Midwife
Heather Simpson, Inflammatory Bowel Disease Specialist Nurse
Issue:
Inflammatory Bowel Disease (IBD) is an Auto-Immune condition that affects the
gastrointestinal system, where the body’s immune system ‘attacks’ healthy cells in the
gut/digestive tract causing it to become inflamed with symptoms. Women with IBD are
at increased risk of adverse pregnancy outcomes, including preterm birth, low birth weight, and
disease flare-ups, particularly when their condition is poorly managed during pregnancy.
The current model of care was fragmented, with women
frequently attending multiple, separate appointments across maternity and IBD clinics leading to delays in specialist input, conflicting medical advice, inefficient
use of resources, and a suboptimal patient experience, increasing the risk of complications and
contributing to patient stress.
Intervention:
The team developed a combined Maternity and IBD Clinic where women were seen by both clinical teams in a single, integrated appointment. By aligning specialist advice, consolidating visits, and enabling real-time interdisciplinary collaboration, the clinic planned to reduce delays in care, enhance the quality of information shared with patients, facilitate prompt interventions, and reduce the number of appointments, therefore patient travel and emissions. The clinic enabled more efficient use of healthcare resources, avoiding unnecessary investigations and potentially costly interventions such as intravenous therapies.
The clinic was designed to use existing clinical templates and appointment slots, minimizing additional cost and avoiding disruptions..
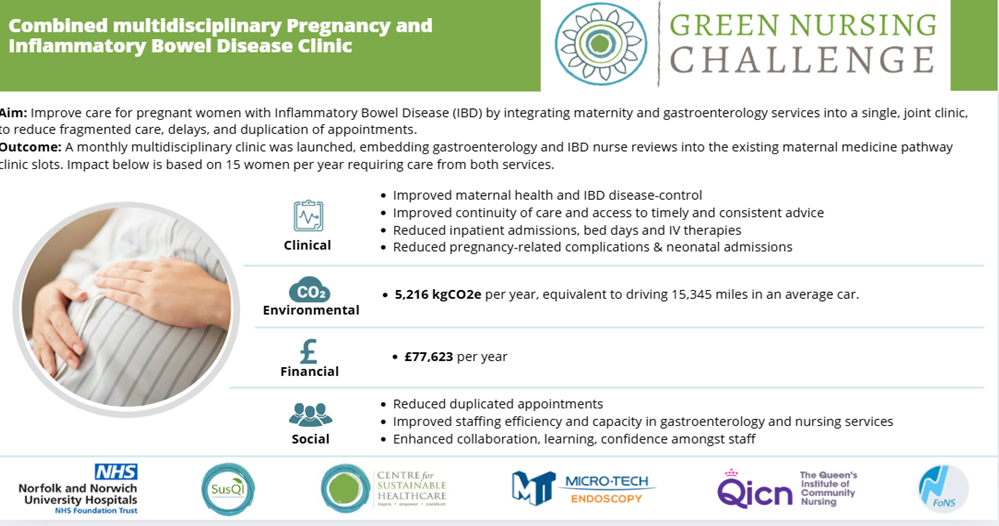
Outcomes:
Clinical
Results showed improvements in maternal & neonatal outcomes through the combined clinic intervention, reinforcing the importance of early assessment and proactive management of IBD in pregnancy. Improved MDT collaboration with the combined clinic led to a greater referral into the
pre-pregnancy counselling service offered by the maternal medicine team, with increased awareness and understanding of the IBD and pregnancy services enabling timely referral through for health optimisation and planning prior to pregnancy.
Results showed a reduced escalation of care in the post-clinic cohort, particularly in terms of higher intervention treatments such as IV steroids and inpatient admissions. In the post-clinic cohort, no patients required inpatient admissions or IV steroids. Results showed that earlier identification and recognition of flare activity through the combined clinic likely led to more timely initiation of treatment.
Findings showed a significant improvement in the quality of antenatal care and risk mitigation in the post-clinic cohort, compared to the pre-clinic model.
Patient feedback highlighted that women felt there was a more cohesive and consistent approach to their care with many valuing the combined expertise and supportive collaborative model.
Environmental
The carbon footprint of 15 pregnant women receiving separate antenatal and IBD care was compared to those seen in the combined clinics, and showed a 51% reduction in emissions - mostly due to reduced medication use (in particular biological IV therapies). Reduced emissions was realised due to a lower neonatal admissions, and patient travel decreased for both hospital and day cases admissions.
With an average of 15 women being seen in the service per year, the projected annual saving were 5215.66CO2e, equivalent to driving 15,345 miles in an average car.
Economical
The combined clinic demonstrated clear cost benefits. The largest cost saving was through fewer inpatient bed stays representing a theoretical cost saving of £42,310.80. In addition, the reduction in medication costs for IV therapies such as Biologics and IV steroids resulted in a combined saving of £8987.92
The cost of providing care to 15 women prior to the change was £95,567.
Following introduction of the joint clinic, this reduced to £17,944, saving £77,623.
Social
The new clinic model allowed women to feel supported by a cohesive team that
offered timely and consistent advice. A combined multidisciplinary approach allowed women to feel that the barriers previously present in accessing specialised care within IBD services were broken down. Access to timely advice and support was notably improved. Women reported feeling listened to and supported in their efforts to achieve a healthier pregnancy. There was a notable improvement in overall confidence following involvement in the Combined Clinic model.
Staff feedback highlighted several key benefits of the combined clinic model:
• Improved continuity of care
• Greater support for pregnant patients with IBD
• Enhanced multidisciplinary collaboration
• Clearer clinical planning and follow-up
Please log in or sign up to comment.